A 75/F with code blue CBBLE UDHC similar cases
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
Chief complaints
Patient came to casualty with unresponsible state with blood pressure not recordable, SPO2 35% on 15 liters of O2 and no pulse with electrical activity.
History of presenting illness
25 yrs ago patient had sudden oncet chest pain, radiating to neck, and palpitations and was taken to hospital and diagnosed to have occlusion myocardial infact and Percutaneous coronary angioplasty was done
2017 patient had complaints of shortness of breath since 2-3 weeks, increased snoring, daytime sleep, which is aggravated , drowsiness since 4 days, pedal edema since 5 days.
Pt was admitted here for further evaluation and management.
Patient was put on Bipap support
2D Echo sh mild concentric LVH, normal LV function, Grade-III diastolic dysfunction.
After stabilization patient was shifted to stepdown ward and treated with sartans, bipap support, antacids nebulization and other supportive care.
During the hospital stay, patient was treated with diuretics, antiplatelets, statins, antibiotics, PPI, oxygen support, NIV support and other supportive care.
Patient was diagnosed with hypertension, Diabetis mellitus, Obstructive sleep a
2022
CPR we started according to 2020 American heart association guidelines and intubated with 7.5 CM ET and bilateral air entry checked cycles of CPR was done with one milligram adrenaline after each cycle
ROSC is obtained after 6 cycles
post CPR vitals
Afebrile
BP 170/100
PR 110 BPM
CVS S1,S2 +
RS BAE+, Decreased air entry in Lt mammary area
Patient is known case of obstructive sleep anea since 2017 is on home by Pep for 3 months patient has settle once it sob at 4:30 p.m. and got relieved with nebulization and 8 a.m. passion and SUV grade 4 taken the local hospital founder to be having blood pressure of 230/110 and was given medications BP reduce to 160/100 with on their way to Hyderabad and patient came and responsive and was bought to our hospital
Patient is on
T. Acebrophylline 200mg + montelukast 10mg H/S
T. Bilatine 20mg H/S
T. Domperidone 30mg + Rabeprazole 20mcg OD
Resp. Budisonide 0.5mg + formoterol 20mcg BD
Home Bipap
Myoclonus
CVS: JVP NORMAL, Apex beat 5th IV space mid clavicular lines1s2 +
RS: BAE + , decreased air entry rt side IMA, IAA, ISA
P/A: soft, non tender , BS +
BGT O POSITIVE
RBS: 211mg/dl
HbA1c : 6.8%
RFT
Blood Urea: 49mg/dl
S. Creatinine: 1.9mg/dl
Na 142
K 4.7
Cl 98
Hemogram
HB 8.5
TC 13,600
MCV 85.9
PCV 27.4
MCH 26.6
MCHC 31
PLT 2.0
P.S NORMOCYTIC, NORMOCHROMIC with neutrophilic leucocytosis
Serum iron : 45ug/dl
ABG post CPR fio2 100%
pH 6.88
PCo2 107
PaO2 77.4
HCO3 1108
SpO2 82.5
ABG day 0 evening fio2 80%
pH 7.46
PCo2 32.8
PaO2 146
HCO3 23.1
SpO2 98.5
ABG day 1 morning fio2 50%
pH 7.43
PCo2 31.9
PaO2 95.3
HCO3 22.6
SpO2 96.8
ABG day 1 morning fio2 40%
pH 7.4
PCo2 31.9
PaO2 80
HCO3 21.5
SpO2 94.7
LFT
TB 0.57
DB 0.16
AST 148
ALT 123
ALP 180
TP 4.7
ALB 2.2
CUE
ALB ++
Sugars nil
Pus cells 4-5
Epithelial cells 1-2
Chest X-ray
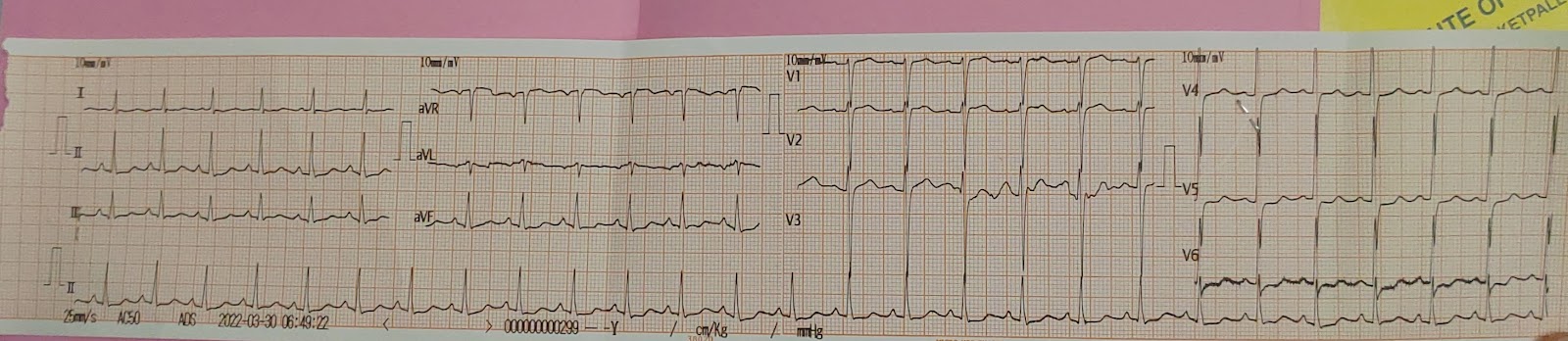
ECG
1-30
Post CPR
2D echo
Concentric LVH
Sclerotic AV
EF 58%
RVSP 35 mmHg
Diastolic dysfunction +
Ventilator settings
Treatment
IVF NS/RL @50ML/HR
Inj. Pan 40 mg IV OD
Inj. Zofer 4 mg IV SOS
Inj. Midazolem titrate B/W 0.1 - 3 mg/Kg
Inj. Atracurium @ 0.8ml/hr (10mcq/hr)
Inj. Levipil 1gm IV STAT
Inj. Levipil 500 mg IV TID
Inj. Clexane 60mg sc OD
RT feeds milk+protein 100ml, water 100ml q4hrly
Propped up position
Air bed with position change 2nd hrly
DAY 1 ECG










Comments
Post a Comment